Elissa Gilbert Miller, MD
Palliative CareResearch Activities
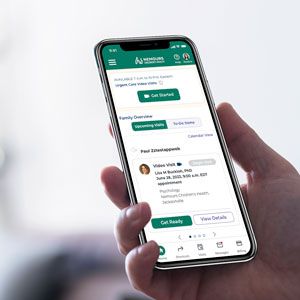
Currently we are taking a look at the place of telemedicine (the use of telecommunication and information technologies to deliver health care at a distance, helping eliminate distance barriers and improving access to medical services) in pediatric palliative care. The goal is to improve pain and symptom management in the home setting and improve patient satisfaction with their caregivers.
We are also looking at the best ways to approach advanced care planning for pediatric inpatients; resource utilization in palliative care; and pain and symptom management in palliative care.
Medical Interests
- Care of children with life threatening conditions
- Care of children with terminal illness
- Pain and symptom management
-
The Landscape of Outpatient Pediatric Palliative Care: A National Cross-Sectional Assessment; Journal of Pain and Symptom Management; (2023).
View Full Publication -
Lessons Learned: Identifying Items Felt to Be Critical to Leading a Pediatric Palliative Care Program in the Current Era of Program Development; Journal of Palliative Medicine; (2021).
View Full Publication -
Palliative Care for Individuals with Cerebral Palsy; Cerebral Palsy; (2020).
View Full Publication -
Palliative Care for Individuals with Cerebral Palsy; Cerebral Palsy: Second Edition; (2020).
View Full Publication -
A Complicated Case of Vaccine Refusal; Pediatrics; (2020).
View Full Publication -
Pediatric Palliative Care; Unknown Source; (2020).
View Full Publication -
Bereavement Accommodations in the Classroom: Experiences and Opinions of School Staff; Journal of School Health; (2020).
View Full Publication -
A Call to Restore Your Calling: Self-Care of the Emergency Physician in the Face of Life-Changing Stress - Part 4 of 6: Physician Helplessness and Moral Injury; Pediatric Emergency Care; (2019).
View Full Publication -
Denying renal transplantation to an adolescent medical cannabis user: An ethical case study; Pediatric Transplantation; (2019).
View Full Publication -
A Call to Restore Your Calling: Self-care of the Emergency Physician in the Face of Life-Changing Stress-Part 1 of 6; Pediatric Emergency Care; (2019).
View Full Publication -
Dyskeratosis Congenita and Oral Cavity Squamous Cell Carcinoma: Report of a Case and Literature Review; Journal of Pediatric Hematology/Oncology; (2019).
View Full Publication -
Palliative sedation with oral medicines in an infant with generalized severe junctional epidermolysis bullosa; Journal of Palliative Medicine; (2018).
View Full Publication -
Palliation in pediatric otorhinolaryngology; International Journal of Pediatric Otorhinolaryngology; (2018).
View Full Publication -
Retrospective review of limitations of care for inpatients at a free-standing, tertiary care children's hospital; Children; (2018).
View Full Publication -
Let's Work Together: Collaborative Research Is Needed to Overcome Difficulty Enrolling Families for Bereaved Sibling Research; Journal of Pain and Symptom Management; (2018).
View Full Publication -
Use of Telehealth in Pediatric Palliative Care; Telemedicine and e-Health; (2017).
View Full Publication -
Pediatric palliative care: Current evidence and evidence gaps; Journal of Pediatrics; (2015).
View Full Publication -
Recent experience establishing a new pediatric palliative care team; Journal of Pediatrics; (2015).
View Full Publication -
Referrals to a new pediatric palliative care team: Details of the first 12 months of operation; Journal of Palliative Medicine; (2014).
View Full Publication -
Cerebral palsy patients discovered dead during sleep: Experience from a comprehensive tertiary pediatric center; Journal of Pediatric Rehabilitation Medicine; (2013).
View Full Publication -
Concurrent care for the medically; Journal of Palliative Medicine; (2012).
View Full Publication
- English
- Spanish